We talked about your Insurance ID card and then gave you some terms you will see on your Explanation of Benefits. Now let’s talk about mistakes. Yes, they happen. Even though physicians and medical providers use electronic medical records, medical billing still relies on people and people make mistakes…
But before we talk about figuring out mistakes, let’s take a look at the process of filing an insurance claim. I think knowing this information can be helpful in figuring out where the mistake might have occurred.
For the sake of this example, let’s make this a fairly easy appointment. You went to your Family Doctor for your annual check-up (you are getting an annual check-up, right? Ok that is probably a whole separate blog post) and during that check-up you have some blood work drawn.
You finish your appointment with the doctor and go check out. You know you owe $35 for the office visit. You pay the co-pay and get your receipt for your payment and leave the office. After you leave, your doctor’s office sends your appointment information to your insurance carrier for payment.
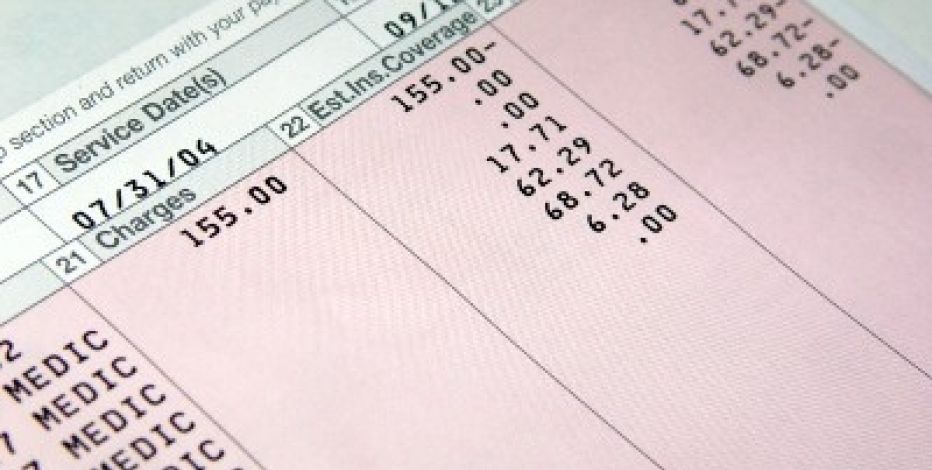
Once your insurance carrier receives the information from your doctor, they then compare your services to your insurance plan to verify how the claim should be paid. Once that process is completed, an Explanation of Benefits is generated for you. On that Explanation of Benefits, information is provided as to how your claim has been paid. It could tell you that you do not owe any additional money to your doctor or that you do have additional responsibilities to pay for that appointment. If you owe additional money, you should receive a bill from your doctor’s office. If your Explanation of Benefit amount and the doctor’s bill match, you should pay your outstanding bill.
Now that is how it is all “supposed” to work. But what if it doesn’t? What if you don’t ever receive an Explanation of Benefits from your insurance carrier? What if you do receive an EOB, but it doesn’t look right? Perhaps it says you owe more than you think you do. With any of these situations, what should be your first step?
- Contact your insurance company. You will need to locate the number on your insurance id card that references billing. Or, if you have an old EOB, look for the phone number that is for questions on that EOB.
- You will need to have your name, your policy id number, group id number, date of the medical appointment and any other receipts or paperwork relevant to that date. Unfortunately, you might have to be on hold for quite a while. Therefore, you want to have everything at your fingertips so you won’t have to call back.
- Depending you what you find out from your conversation, you might have to have your doctor resubmit the claim or the insurance company to reprocess the claim. Either way, do not pay the doctor until all questions have been answered and the claim has been processed correctly.
If this all sounds way too complicated and frustrating and you are a client of Cancer Patient Services, please reach out to us. We would be happy to work through these issues on your behalf. Call us at 419-423-0286 to make an appointment.
We found this Consumer Reports article to be helpful in decoding medical billing errors.


 RSS Feed
RSS Feed

